Arslan, Çağatay
Loading...

Profile URL
Name Variants
Arslan, C.
Arslan, C
Arslan, Cagatay MD
Arslan, Çagatay
Arslan, Cagatay
Arslan, Ç
Arslan, C
Arslan, Cagatay MD
Arslan, Çagatay
Arslan, Cagatay
Arslan, Ç
Job Title
Email Address
cagatay.arslan@ieu.edu.tr
Main Affiliation
09.02. Internal Sciences
Status
Current Staff
Website
ORCID ID
Scopus Author ID
Turkish CoHE Profile ID
Google Scholar ID
WoS Researcher ID
Sustainable Development Goals
8
DECENT WORK AND ECONOMIC GROWTH

0
Research Products
9
INDUSTRY, INNOVATION AND INFRASTRUCTURE

0
Research Products
10
REDUCED INEQUALITIES

0
Research Products
17
PARTNERSHIPS FOR THE GOALS

0
Research Products
12
RESPONSIBLE CONSUMPTION AND PRODUCTION

0
Research Products
7
AFFORDABLE AND CLEAN ENERGY

0
Research Products
1
NO POVERTY

0
Research Products
5
GENDER EQUALITY

0
Research Products
13
CLIMATE ACTION

0
Research Products
4
QUALITY EDUCATION

0
Research Products
14
LIFE BELOW WATER

0
Research Products
2
ZERO HUNGER

0
Research Products
15
LIFE ON LAND

0
Research Products
16
PEACE, JUSTICE AND STRONG INSTITUTIONS

0
Research Products
6
CLEAN WATER AND SANITATION

0
Research Products
3
GOOD HEALTH AND WELL-BEING

14
Research Products
11
SUSTAINABLE CITIES AND COMMUNITIES

0
Research Products

Documents
126
Citations
2340
h-index
23

Documents
73
Citations
580

Scholarly Output
34
Articles
24
Views / Downloads
27/48
Supervised MSc Theses
0
Supervised PhD Theses
0
WoS Citation Count
317
Scopus Citation Count
303
WoS h-index
6
Scopus h-index
6
Patents
0
Projects
0
WoS Citations per Publication
9.32
Scopus Citations per Publication
8.91
Open Access Source
14
Supervised Theses
0
| Journal | Count |
|---|---|
| Annals of Oncology | 5 |
| Clinical Genitourinary Cancer | 4 |
| Journal of Clınıcal Oncology | 2 |
| Cancer Medicine | 1 |
| Cancer treatment reviews | 1 |
Current Page: 1 / 6
Scopus Quartile Distribution
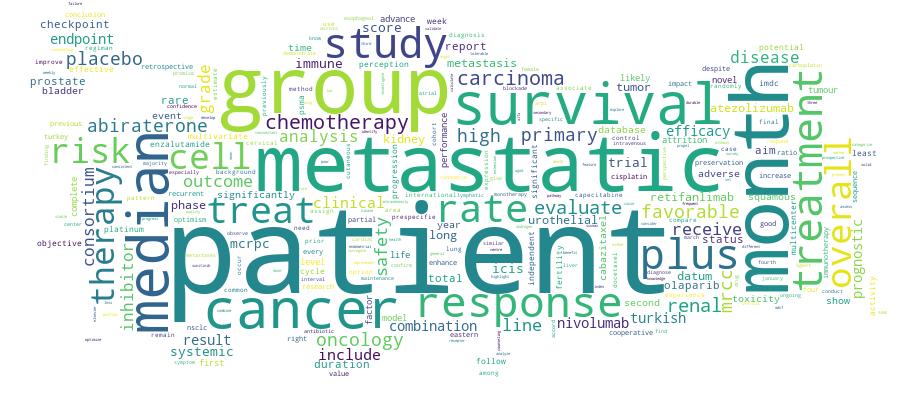
Competency Cloud
34 results
Scholarly Output Search Results
Now showing 1 - 10 of 34
Conference Object Citation - WoS: 10Biomarker Analysis and Updated Results From the Phase Iii Propel Trial of Abiraterone (abi) and Olaparib (ola) Vs Abi and Placebo (pbo) as First-Line (1l) Therapy for Patients (pts) With Metastatic Castration-Resistant Prostate Cancer (mcrpc)(Elsevier, 2022) Saad, F.; Armstrong, A. J.; Thiery-Vuillemin, A.; Oya, M.; Shore, N. D.; Procopio, G.; Arslan, C.[Abstract Not Available]Article Enhancing Outcomes in mCRPC: The Impact of Androgen Receptor Inhibitor Sequencing Before 177Lu-PSMA Therapy(Oxford Univ Press, 2025) Yazgan, Sati Coskun; Kayas, Kamil; Arslan, Cagatay; Kapar, Caner; Oztekin, Sura; Ceylan, Furkan; Urun, YukselBackground Prostate-specific membrane antigen (PSMA) is a key target in metastatic castration resistance prostate cancer (mCRPC). Enzalutamide, an androgen receptor pathway inhibitor (ARPi), increases PSMA expression, potentially enhancing 177Lu-PSMA-617 radioligand therapy. This study evaluates the impact of prior ARPi (enzalutamide vs abiraterone acetate [AA]) on PSMA expression, PFS, and OS. Materials and Methods A retrospective analysis of 214 mCRPC patients treated with 177Lu-PSMA-617 across six Turkish centers (2015-2025) was conducted. Patients were grouped by prior ARPi therapy. PFS and OS were analyzed using Kaplan-Meier and Cox regression methods. Results Among 103 patients receiving ARPi before 177Lu-PSMA-617, 59 (57%) had enzalutamide and 44 (43%) AA. Median PFS was 7.6 months for enzalutamide versus 5.3 months for AA (P = .068). Median OS was significantly longer with enzalutamide (12.8 vs 6.9 months, P = .021). Patients with Eastern Cooperative Oncology Group Performance Scores (ECOG PS) 0-1 had significantly longer OS (27.6 vs 6.9 months for PS 2-3, P < .0001). Higher PSMA SUVmax (>20) correlated with longer OS (15.1 vs 7.8 months, P = .016). Among 86 patients with detectable PSMA SUVmax, 53 had SUVmax > 20; 66% had prior enzalutamide and 34% AA. Median OS was four months longer with enzalutamide (18.1 vs 13.9 months P = .120). Multivariate analysis identified ARPi type (HR: 2.24, P = .033) and ECOG PS (HR: 5.22, P < .0001) as independent OS predictors. Conclusion Enzalutamide prior to 177Lu-PSMA-617 significantly improves OS and enhances PSMA expression compared to AA. These findings highlight the importance of treatment sequencing in mCRPC and warrant further prospective studies.Article Treatment Patterns and Attrition in Metastatic Renal Cell Carcinoma: Real-Life Experience From the Turkish Oncology Group Kidney Cancer Consortium (tkcc) Database(Cig Media Group, Lp, 2024) Bolek, Hatice; Sertesen, Elif; Kuzu, Omer Faruk; Tural, Deniz; Sim, Saadet; Sendur, Mehmet Ali Nahit; Urun, Yuksel; Arslan, CagatayThe inclusion of patients with more favorable prognoses in clinical trials imits generalizability to broader and more diverse patient group. This study examines treatment patterns and attrition rates in Turkish oncology clinics for metastatic renal cell carcinoma. The percentages of patients receiving treatment in the second, third, and fourth lines of therapy were 62.8%, 27.4%, and 8.9%, respectively. Disease progression was the primary cause of attrition, followed by toxicity. Introduction: Despite the rapid evolution in management of metastatic renal cell carcinoma (mRCC) over the past decade, challenges remain in accessing new therapies in some parts of the world. Despite therapeutic advancements, attrition rates remain persistently high. This study aims to assess the treatment patterns and attrition rates of patients with mRCC in oncology clinics across Turkey. Patients and Methods: Patients diagnosed with mRCC between January 1, 2008, and December 31, 2022, with first-line systemic treatment data, were retrospectively evaluated using the Turkish Oncology Group Kidney Cancer Consortium (TKCC) Database. Results: The final analysis included a total of 1126 patients. The percentages of patients treated in the 2nd, 3rd, 4th, and 5th lines of therapy were 62.8%, 27.4%, 8.9%, and 2.1%, respectively. The drugs that were most commonly used in the groups were tyrosine kinase inhibitors (TKIs) (52.2%) and interferon (IFN)-alpha (43.3%) for the first line, TKIs (66.3%) and immunotherapy (IO) monotherapy (25.9%) for the second line, TKI (41.4%) and mTOR inhibitors (28.8%) for the third line, TKI (44.4%) and mTOR inhibitors (29%) for the fourth line, and IO monotherapy (37.5%) and TKI (25%) for the fifth line. For the first-line treatment, the primary cause of attrition was disease progression (66.4%), followed by toxicity (16.5%), death (11.2%), and patient preference (5.9%). The primary reason for attrition across all treatment lines was disease progression. Over time, the use of TKIs in first-line treatment increased, while IFN-alpha usage declined. IOs began to be utilized in earlier lines, predominantly in second-line treatment, though use of IO-based combination therapies remains limited. Conclusion: This study underscores that despite significant progress in therapeutic options, the adoption of novel agents remains slow, and attrition rates are still high. These findings indicate a disparity in systemic therapy compared to developed countries.Conference Object Long-Term Outcome and Safety in Patients Treated With Immune Checkpoint Blockade Therapies for Urothelial Carcinoma: Experience From Real-World Clinical Practice.(Lippincott Williams & Wilkins, 2022) Tural, Deniz; Arslan, Cagatay; Selcukbiricik, Fatih; Olmez, Omer Fatih; Erman, Mustafa; Urun, Yuksel; Karadurmus, Nuri[Abstract Not Available]Article The Efficacy of Immunotherapy and Chemoimmunotherapy in Patients With Advanced Rare Tumors: a Turkish Oncology Group (tog) Study(Wiley, 2023) Güven, Deniz Can; Aykan, Musa Barış; Muglu, Harun; Bayram, Ertuğrul; Helvacı, Kaan; Dursun, Bengue; Celayir, Melisa; Arslan, ÇağatayIntroduction: The advances in immune checkpoint inhibitors (ICIs) were relatively slow in rare tumors. Therefore, we conducted a multi-center study evaluating the efficacy of ICI monotherapy and the combination of ICIs with chemotherapy (CT) in patients with advanced rare tumors.Methods: In this retrospective cohort study, we included 93 patients treated with ICIs for NCI-defined rare tumors from the 12 cancer centers in Turkey. The primary endpoints were the overall response (ORR) and disease control rate (DCR).Results: The cohort's median age was 56, and 53.8% of the patients were male. The most frequent diagnosis was sarcoma (29%), and 81.7% of the patients were previously treated with at least one line of systemic therapy in the advanced stage. The ORR and DCR were 36.8% and 63.2%, respectively. The germ cell tumors had the lowest ORR (0%), while the Merkel cell carcinoma had the highest ORR to ICIs (57.1%). Patients treated with ICI + ICI or ICI plus chemotherapy combinations had higher ORR (55.2% vs. 27.6%, p = 0.012) and DCR (82.8% vs. 53.4%, p = 0.008). The median OS was 13.47 (95% CI: 7.79-19.15) months, and the six and 12-month survival rates were 71% and 52%. The median duration of response was 16.59 months, and the 12-month progression-free survival rate was 66% in responders. The median time-to-treatment failure was 5.06 months (95% CI: 3.42-6.71). Three patients had high-grade irAEs with ICIs (grade 3 colitis, grade 3 gastritis, and grade 3 encephalitis in one patient each).Results: The cohort's median age was 56, and 53.8% of the patients were male. The most frequent diagnosis was sarcoma (29%), and 81.7% of the patients were previously treated with at least one line of systemic therapy in the advanced stage. The ORR and DCR were 36.8% and 63.2%, respectively. The germ cell tumors had the lowest ORR (0%), while the Merkel cell carcinoma had the highest ORR to ICIs (57.1%). Patients treated with ICI + ICI or ICI plus chemotherapy combinations had higher ORR (55.2% vs. 27.6%, p = 0.012) and DCR (82.8% vs. 53.4%, p = 0.008). The median OS was 13.47 (95% CI: 7.79-19.15) months, and the six and 12-month survival rates were 71% and 52%. The median duration of response was 16.59 months, and the 12-month progression-free survival rate was 66% in responders. The median time-to-treatment failure was 5.06 months (95% CI: 3.42-6.71). Three patients had high-grade irAEs with ICIs (grade 3 colitis, grade 3 gastritis, and grade 3 encephalitis in one patient each).Conclusion: We observed over 30% ORR and a 13-month median OS in patients with rare cancers treated with ICI monotherapy or ICI plus CT combinations. The response rates to ICIs or ICIs plus CT significantly varied across different tumor types. Responding patients had over 2 years of survival, highlighting a need for further trials with ICIs for patients with rare tumors.Conference Object Romiplostim for Chemotherapy-Induced Thrombocytopenia (cit) in Solid Tumors: Two Phase Iii, International, Randomized Controlled Trials (rct)(Elsevier, 2022) Al-Samkari, H.; Geredeli, C.; Arslan, C.; Korantzis, I.; Dogu, G. G.; Nechaeva, M.; Salgado Fernandez, M.[Abstract Not Available]Conference Object Real-Life Experience With Chemotherapy Plus Biologics in First-Line Treatment of Right-Sided, Ras Wild-Type, Metastatic Colon Cancer: a Multicenter Onco-Colon Turkey Study(Elsevier, 2021) Arslan, Çağatay; Kefeli, U.; Yildirim, E.; Isikdogan, A.; Karadurmus, N.; Karabulut, B.; Cicin, I.[Abstract Not Available]Conference Object Citation - WoS: 1Two Randomized Controlled Trials of Romiplostim for Chemotherapy-Induced Thrombocytopenia in Patients With Solid Tumors(Amer Soc Hematology, 2022) Al-Samkari, Hanny; Geredeli, Caglayan; Arslan, Cagatay; Korantzis, Ippokratis; Dogu, Gamze Gokoz; Nechaeva, Marina; Fernandez, Mercedes Salgado[Abstract Not Available]Conference Object Real-World Treatment Outcomes From Nationwide Onco-Colon Turkey Registry in Ras Wild-Type Patients Treated With Biologics First-Line Metastatic Colorectal Cancer.(Lippincott Williams & Wilkins, 2021) Kefeli, Umut; Arslan, Cagatay; Yildirim, Mahmut Emre; Isikdogan, Abdurrahman; Karadurmus, Nuri; Karabulut, Bulent; Cubukcu, Erdem[Abstract Not Available]Article Citation - WoS: 1Citation - Scopus: 2Cutaneous Metastasis of Bladder Urothelial Carcinoma; a Rare Conditions(Elsevier Science Inc, 2022) Oztuerk, Hakan; Yurtsever, Selin; Ozer, Arzum; Arslan, Cagatay; Tekeli, Aysun; Pehlivan, Fatma SeherCutaneous is an extremely rare metastatic area of bladder urothelial carcinoma. Pure cutaneous metastasis without systemic metastasis is very rare and less than ten cases have been reported in the literature. Our patient had various lymphatic fistulas to her skin due to pelvic lymphadenectomy and radiotherapy in her previous cervical cancer. We believe that the most probable mechanism underlying our patient's cutaneous metastasis is a lymphatic spread via those lymphatic fistulas. Immunotherapy is a very important option for patients who cannot receive cisplatin. This is the second case in the literature to apply immunotherapy in the setting of cutaneous metastasis of bladder cancer.

